
- No win. No fee.
- No hidden costs
- 100% risk-free, only pay if you win
- Home >
- Insights >
- Misdiagnosis Claims >
- Knowing the risks of Deep Vein Thrombosis (DVT) misdiagnosis
About the Author
Tami Frankel
Medical Negligence Solicitor and Partner - LLB (Hons) University College London
Read more about Tami »Due to the extensive training undertaken by doctors, nurses and other medical professionals, DVT misdiagnosis is a rare occurrence. But, the human body is very complex, and what can appear on the surface as a simple leg cramp or a muscle strain could actually be something far more serious and, in some cases, life-threatening.
An example of this is Deep Vein Thrombosis (DVT). DVT can present with symptoms that are common for a number of conditions, and can also be present with no symptoms at all. This can lead to a delay in diagnosing DVT which carries a great deal of risk.
In 2009, it was estimated that 40,000 deaths in England per year were a result of complications caused by DVT. Furthermore, these findings estimated that around 25,000 of these deaths could have been prevented if not for misdiagnosis or inefficient treatment.
Since then, the NHS and other medical bodies have taken strides in reducing the incidence of hospital-related harm caused by DVT, with a 20% drop in the number of post-discharge deaths between 2008 and 2019. However, it is believed this still occurs in 57 of every 100,000 cases, and these can often be due to a medical misdiagnosis.
In this article, as specialist and experienced DVT negligence solicitors, we will break down what Deep Vein Thrombosis is and why it is important to assess quickly, why there is the potential for DVT misdiagnosis, and what you can do if the consequences of your DVT are the result of medical negligence.
The consequences of DVT misdiagnosis
What is DVT?
Deep Vein Thrombosis is when a blood clot forms in one of the deep veins within the body. These are typically known to occur in the leg, but can also occur in the arms or pelvis. It is estimated that 1 in 1,000 people each year will get DVT.
What are the warning signs of a blood clot in your leg?
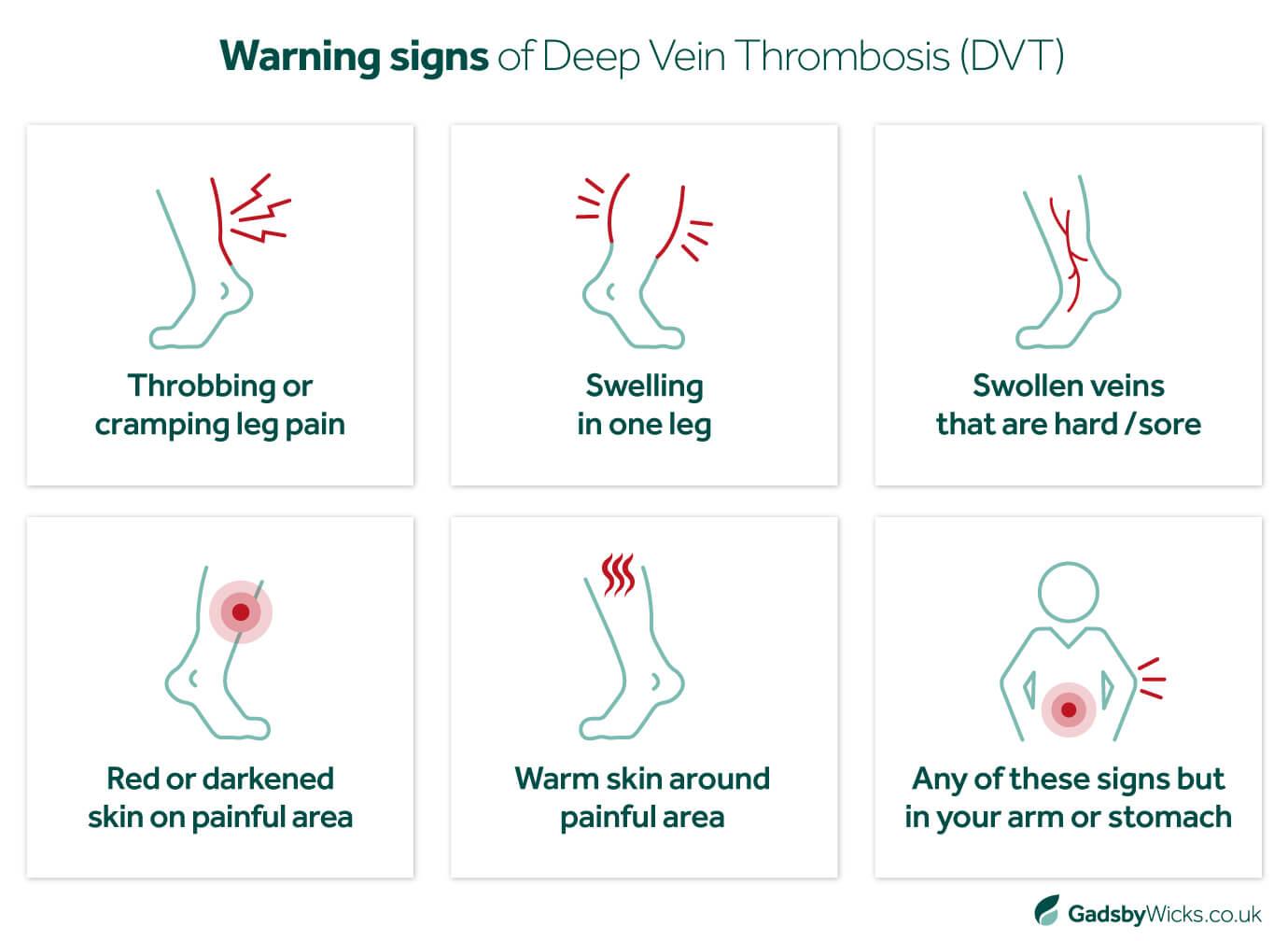
However, it is possible for DVT to present with no symptoms or pain whatsoever, making it difficult for people to recognise or diagnose. This means in order to minimise the risk of a DVT misdiagnosis, medical professionals need to take into account the various risk factors that make the possibility of Deep Vein Thrombosis more likely.
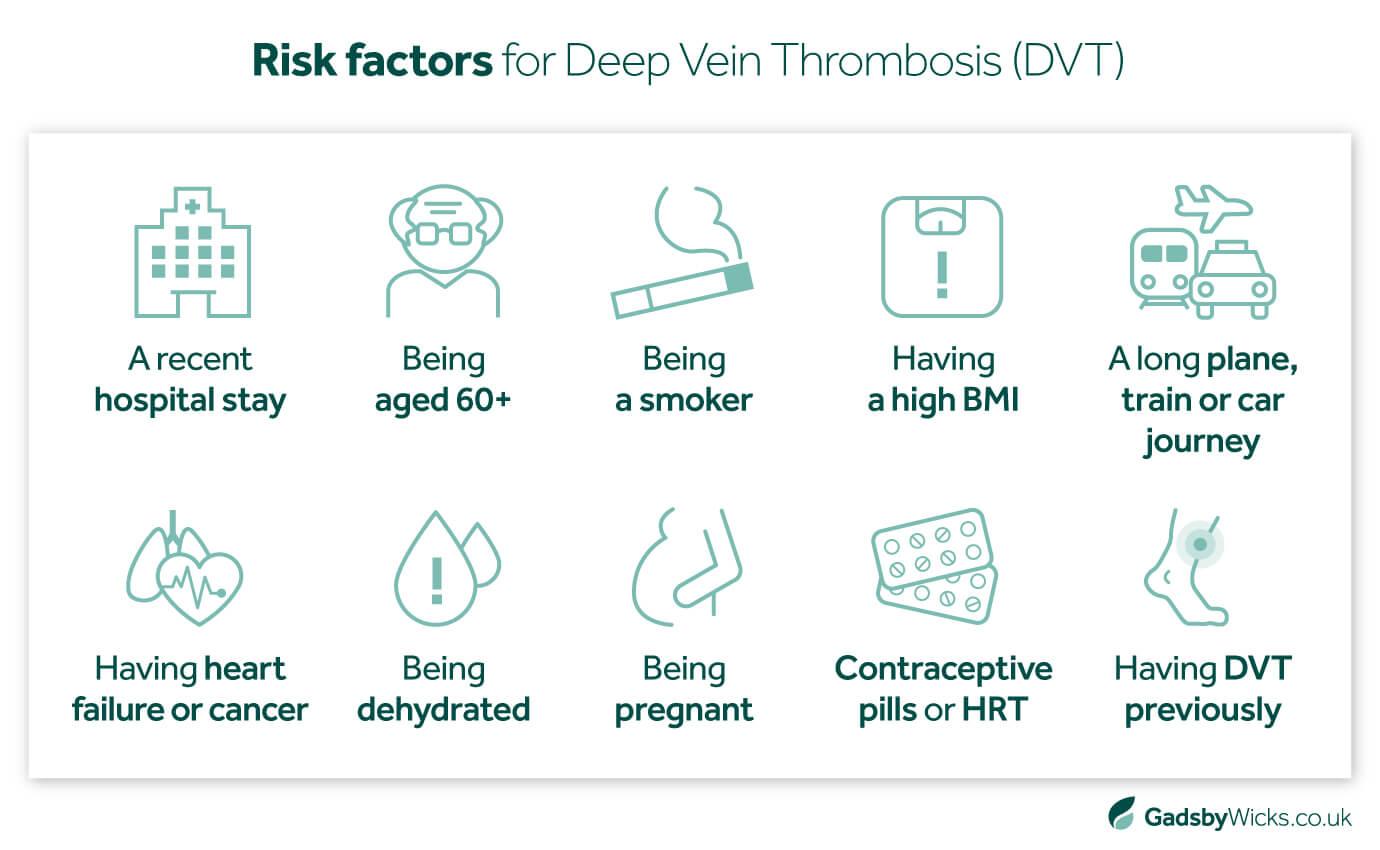
The risk of Deep Vein Thrombosis depends on a number of factors, including:
How long can you have DVT without knowing?
Listening to your body and identifying any of the signs or symptoms listed earlier will be vital in knowing whether you have a DVT.
If a DVT is related to a journey or sitting still for a long period of time, the symptoms can develop after a few hours or even days later. The best thing you can do is take preventative measures and keep yourself moving on long journeys or during extended periods of sitting.
When the symptoms appear, they are usually sudden, so ensure you get medical help as soon as you identify anything out of the ordinary. Likewise, the severity of symptoms will differ between individuals, so speak to your GP as soon as you can. If you can’t reach your GP and suspect you have a DVT, you should call 111 or go to your nearest emergency department.
You can explore more of the causes of Deep Vein Thrombosis on the NHS website. But it is important to note that there can be situations where DVT happens without any identified cause, again making it essential that any sign of DVT is taken seriously by healthcare professionals so, if identified, it can be treated as soon as possible.
That is because, if left untreated, complications of Deep Vein Thrombosis can lead to other serious and potentially life-threatening conditions, such as:
Pulmonary Embolism
A pulmonary embolism is when a blood clot reaches the lungs causing shortness of breath, chest pains, fainting and other symptoms. If this blocks oxygen from entering the lungs for too long, a pulmonary embolism can easily prove fatal.
Post-Phlebitic Syndrome (post-thrombotic syndrome)
Damage caused by DVT can reduce the flow of blood to the affected area, known as Post-Phlebitic Syndrome or Post-Thrombotic Syndrome, which can lead to persistent swelling of the legs, development of leg ulcers, discolouring of the leg, and other ongoing, painful symptoms.
In severe cases or when not treated quickly enough, DVT can also result in the need for amputation of the affected limb, or the development of long-term conditions like varicose veins.
Misdiagnosis of DVT due to negligence can have significant consequences. It is estimated that an untreated DVT carries a 30% risk of death, whereas, with treatment, the risk falls to between 2% and 8%. Anyone affected by a negligent delay in treating or diagnosing a DVT can claim compensation for the injury caused to them by that delay.
How can DVT be misdiagnosed?
Because the symptoms of DVT are commonly experienced and not necessarily specific to DVT, it is possible to misdiagnose DVT. There have been numerous cases of DVT being misdiagnosed as sciatica, muscle strains or even cramp.
While these incidents are thankfully rare, this potential for misdiagnosis means that it is important for healthcare professionals to consider the possibility of DVT even in low-risk scenarios. NICE (The National Institute of Health and Care Excellence) has developed guidelines to help professionals assess the risk of someone having DVT.
If a healthcare professional believes there is a risk of their patient suffering a DVT, they should run necessary tests to verify this. After an initial examination and wellness check, in most cases testing for DVT will begin with a D-Dimer blood test. This measures the amount of fibrin in your blood, a substance that develops when a clot is broken down. A negative test means a clot is unlikely.
Should the D-Dimer be positive or inconclusive, your doctor should then perform a Doppler ultrasound. This scans your leg or other affected area, identifying areas where blood flow starts and stops. If the flow indicates that there is some form of blockage, this can again indicate the presence of a clot.
In some circumstances, the patient may receive an MRI or venogram (a special type of X-ray) if the clot is located somewhere other than the leg or if other tests prove inconclusive. However, this is uncommon due to the costs and inconvenience involved with these procedures.
As noted earlier, there is a close correlation between patients who had extended stints in hospital and cases of DVT. Thrombosis UK even claims that VTE is the leading cause of preventable deaths in hospitals, with someone dying of this condition in the western world every 37 seconds.
Therefore it is critical that healthcare professionals take the necessary steps to review and assess patients who are bed-bound for a length of time to determine their risk of developing DVT in the weeks following their treatment. Steps that can be taken to prevent DVT include:
- Providing anticoagulant medicine during your stay, which will thin the blood and therefore reduce the risk of any clots forming in deeper veins
- Encouraging you to wear compression socks or stockings during the patient’s stay and afterwards, as these will help to improve circulation in their legs
- Advising on walking and further exercise when the patient is back on their feet, to reduce the risk of clots forming if they remain inactive
- Suggesting exercises that patients can do in bed, like ankle rolls and elevating their legs, in order to continue circulation if they can’t walk for a while
It is the duty of healthcare professionals to take all expected precautions for patients who may be at risk from DVT; failure to identify this risk or negligence in actually applying said steps can put the health of the patient at risk.
Pursuing a claim for misdiagnosed DVT
While more diligent processes have greatly reduced the potential of DVT misdiagnosis, mistakes do still happen and, if they do, the consequences may be severe. We understand how the failure to identify DVT promptly can lead to tragedy for the affected person and their loved ones, which is why we strive to support them in any way we can.
As deep vein thrombosis claims experts, we have supported many clients who have been affected by a medical misdiagnosis from a professional they believed they could trust, working closely with them to secure the answers, compensation and justice they are owed.
Our highly qualified and experienced medical negligence solicitors are meticulous in their approach to investigating any case, ensuring you are clear on whether you have a medical malpractice claim and the steps needed to achieve the result you deserve.
Get in touch with us today to discuss your situation and whether you have a DVT negligence claim.
Disclaimer
All content contained within this article is meant for general information only – this should not be treated as a substitute for medical advice from your doctor or another healthcare provider. If you require legal advice specific to your situation, please contact our team directly.
Gadsby Wicks is not liable for any diagnosis made from the content of this article, nor does it endorse any service or external site linked to within the article.
Always consult your GP if you are concerned about your health and wellbeing, or speak to us if you require legal advice.




 Back to top
Back to top
